I woke up and my feet hurt as soon as I got out of bed…
Did it ever happen to you that your feet hurt right when you got up in the morning? It did to me, when I was about seven months pregnant. One day when I stepped out of bed I winced because my feet really hurt – right after they had been resting all night long. Interestingly, while going through the morning routine, which always involves some walking about, the pain evaporated, and I thought no more of it.
Until the next morning, when the same thing happened. I had slept well all night, my feet were rested – and yet, as soon as I put my weight on them that pain shot through my soles again. Again, it went away after spending some time on my feet doing my routine morning activities. And if I remembered that strange pain at all, it was only to be glad that it had gone away.
But it was back again the next day, and I knew I had to find out what was going on. Especially, when I spent a block of several hours sitting down, and found my feet yet again painful on rising. As you might know by now, I detest bothering a busy doctor with someone I can do for myself. So off I went to the greatest collection of knowledge the world has ever known – to which I happen to have access from my own living room. And I found out about a condition called “plantar fasciitis”.
I. Symptoms of and general risk factors for plantar fasciitis
The mayo clinic describes the symptoms of plantar fasciitis as “a stabbing pain in the bottom of your foot near the heel” that “usually occurs with your first steps in the morning. As you get up and move, the pain normally decreases, but it might return after long periods of standing or when you stand up after sitting”.
Bingo! That was exactly what I had been experiencing. Except the pain had not been restricted to the base of the heel, most of my sole hurt.
So who is at risk for developing this strange foot condition? The Mayo Clinic answers that
plantar fasciitis is more common with age (especially between the ages of 40 and 60), in runners and dancers (since their activities strain heels and attached tissues more), in overweight people, in people with jobs that keep them on their feet walking or standing on hard surfaces, as well as those who have either over-pronated (flat) or under-pronated (high-arched) feet and wear shoes with inadequate support or cushioning. Pronation is about the movement your foot makes when walking or running, and unbalanced movement over large distances and on hard surfaces can cause injury, including plantar fasciitis.
Again – bingo! I was pregnant and had rapidly gained about 20 kg over the span of only four months or so.
Not that I was worried about the weight gain, since I was on a diet (the only one I’ve ever been on). This “Bradley diet” calls for healthy food intake with at least 80g of protein a day in order to do proper “body building”. This was the fourth body I was building, and I knew how important proper diet is for good results. Besides, weight gained through healthy eating in pregnancy is easily gotten rid of through birth and breastfeeding. But all that is a topic for another day.
If you are wondering whether you may have overpronated feet you can check the soles under your shoes. If the outer side of the heels of your soles are wearing out much faster than the inner sides, chances are you have overpronated feet. After all, the great Doctor Mandell says that this condition has become a major epidemic.
At first I wondered whether there was some mistake here – I would have though wearing on the inner soles would indicate over-pronation. And I’m not the only one – I found a lot of contradictory information on the web. But Footminders’ photos convinced me – their picture sequence on the right demonstrates how a flat-footed person walks: notice that the heel normally strikes on the outside first, and then afterwards the feet roll inwards as part of normal walking motion. In many cases, the more a person lands on the outside edge of their feet, the more their feet will roll inwards. This lateral instability results in wear not only on the heels outer and back edges, but also on the inner ball areas of the forefoot. Shoes with more support can be helpful for these over-flexible feet.
The shoe soles of high-arched under-pronators (also called supinators) do show wear on the outside of the soles, as well, but this wear will extend beyond the heels and manifest under the forefoot of the shoe. Since the feet of under-pronators are essentially too rigid, they will benefit from shoes with extra cushioning.
Of course I looked at my own shoe soles, and found that while I did have quite some wear in the outer heel area, the rest of the wear was right in the middle of the ball area. Footminders says that it’s normal for our feet to land on the outside edge of our heel first (heel strike) – so I guess that means I’m good. My husband, however, shows the typical over-pronation pattern – wear in both the outer and back edges of the heel.
What on earth are fasciae?
Back to plantar fasciitis – what is it, and why would weight gain (or running, or working all day on your feet on hard floors) cause such a strange pattern of foot pain? I mean, I can understand my feet hurting from the extra weight after being up and about all day – but why the pain right after resting my feet all night long?
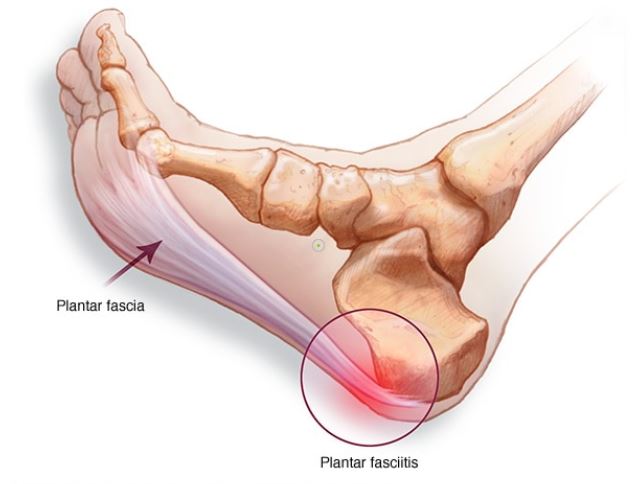
In order to answer these questions it’s important to look at the anatomy involved in the problem. Plantar fasciitis affects a dense, fibrous band of tissue (called the plantar fascia) that runs across the bottom of the feet in order to connect the heel bone to the base of the toes. For this reason it can be called a ligament. Ligaments join one bone to another (tendons, on the other hand, join muscle to bone). But the name “plantar fascia” has stuck. Fasciae are usually understood to be thin sheets of tissue similar to cling-film that envelope , separate, or bind together muscles, organs and other tissues of the body, including blood vessels and nerves, keeping everything in its proper place. Without them the body would be a rather loose mass of skin, bones and other parts. The fascial system has been described as a “3-D spider web of fibrous, gluey, and wet proteins” that bind together the seventy trillion cells that make up our bodies. Since ligaments share this function and consist of the protein (collagen) they have been defined as part of the fascial system, which in turn is part of the extra cellular matrix.
I had never heard of this important system before – no doubt because (according to a German study) they have been pretty much overlooked in mainstream medicine, and their contribution to many areas of biomechanics and physiology has been underestimated. One huge reason for this is anatomical science’s preoccupation with reductionism. By dissecting bodies with the scalpel, scientists have learned a great deal about the separate parts of our anatomy. We now know that the average adults has 208 bones in his body. But fasciaes aren’t that easy to count, since “the fascial body seems to be one large networking organ, with many bags and hundreds of rope-like local densifications, and thousands of pockets within pockets, all interconnected by sturdy septa as well as by looser connective tissue layers”, as the study explains. Is lies in the nature of things that dissection does not help the understanding of how everything in the body is connected. And so the role of the body’s fascia system in overall health as the integrater of posture and movement with great influence on other body systems has only recently begun to be appreciated by science. Massage therapists, physiotherapists, acupuncturists, and other healthcare providers, however, have long recognized the importance of the fascial system; this is usually where any kind of movement therapy begins.
As an interesting linguistic aside, the word fascia comes from the latin for “band, bandage” – which is related to fasces (a bundle of rods with a projecting axe blade, used in both ancient Rome and Fascist Italy as a symbol of governmental authority). The common idea is that in a fascia the band of tissue runs in a certain direction, while the rods in the fasces are bundled in the same direction. Accordingly, in fascism the dictatorial power forces all opposition into cooperating with its own direction of action, in order to unite society and economy into one strong force.
But this is meant to be a health article, so back to the plantar fascia. According to other recent studies, this fascia should be reclassified as an “aponeurosis”. Well, so I just learned that an aponeurosis is a ribbon of pearly white fibrous tissue (due to being little supplied with blood vessels and nerves) that takes the place of a tendon in flat muscles with a wide area of attachment (as can be seen in the photo). I guess it’s true that no other area of anatomical science has such divergent terminology as this one! But I’ll continue to use the well-known name “plantar fascia”.
The plantar fascia is in the shape of a bowstring, and supports the arch on the bottom (plantar side) of the foot. The plantar side is the side you plant onto the ground, so to speak. It mainly consists of longitudinally oriented collagen fibers, made to absorb shock from walking, running and jumping.
Interestingly, in younger people the plantar fascia is intimately related to the Achilles tendon, but the continuity of this connection decreases with age to a point where in elderly people there are few connecting fibers left.
What causes feet to hurt after resting all night?
Although the plantar fascia is made to support a lot of weight, too much stress through overuse, repeated straining and especially injury such as tearing will irritate and inflame the plantar fascia, and then you have plantar fasci-itis (just like the condition of an inflamed appendix is called appendic-itis, or inflamed bronchia – bronch-itis).
In my case, rapid weight gain due to pregnancy had strained my plantar fasciitis’ ability to adapt. An older friend of mine developed plantar fasciitis after she started a new job that all of a sudden required much more standing than her feet had been used to.
The irritated fascia will contract, tighten, and shorten in an effort to grow stronger and manage the added stress. Stretching opposes this contracting and therefore is painful. When your feet have been resting all night, your inflamed plantar fasciae have remained in a contracted position for hours on end. Then, when your soles contact the floor in the morning and get your full weight placed upon them, the plantar fasciae are stretched very suddenly and this is what causes that pain.
Interestingly, the effects of plantar fasciitis can go much further than simply experiencing pain in the soles on rising. Since the fascial system is completely interconnected, tight soles can cause knee, hip and back problems. They can cause problems as far away as the jaws! The Bristol Massage Clinic explains that one of twelve lines of myofascial chains that runs through the body is the “Superficial Back Line”, which starts at the soles of our feet, continues up and over the top of our head, and ends at the brow ridge. If you imagine this line as a set of muscles wrapped entirely in cling film (fasciae), it’s easy to see how pulling on one part of this chain would pull elsewhere down the line. When any area of this fascia in between your feet and head gets irritated or loses its functional capacity, the body will compensate. Thus, irritated soles can affect how someone chews or holds their jaw.
This should make it extra clear that you can’t just tough it through the first minutes of the day, waiting for the pain to go away and then ignore the problem. You must take care of it.
II. How can I heal my plantar fascia?
Once we understand what plantar fasciitis actually is and what causes it, it isn’t hard to find self-help options.
1. Reduce risk factors!
First of all, relevant risk factors need to be removed as much as possible (such as loosing weight, finding shoes with good foot support, spending less time on your feet or arranging for a more springy surface to stand on during work, instead of hard concrete only).
In my case it was obvious that I needed to loose weight – which was easily accomplished by giving birth a couple months later (and yes, I do mean it was an easy birth in the peace of my own home, with the baby alone weighing over 4kg – but again, that’s for another article).
If you have “other weights” to shed you could look into intermittent fasting (it has done wonders for both my sister and my husband), and I very much recommend looking into how else you might change your diet and lifestyle to accomplish healthy weight loss. I’ll have to write about this another time.
2. Get off your feet periodically to rest them!
Next, you must rest your feet more to give those fasciae a chance to heal. I have read it recommended to wear stiff-soled shoes (such as hiking boots) to avoid stressing the plantars when you do have to keep standing and walking. Personally I didn’t try this – instead, I wore Birkenstock shoes around the house, which are known for their arch support design. They really do feel good.
3. Stretch those plantar fasciae!
Finally, since the problem involves tightened fasciae, it’s key to work on stretching them, as well as the Achilles tendon and the calves. I have read of dorsiflexion night splints for sleeping (to passively keep the fasciae stretched), and of taping the arch of the foot (recommended for dancers), but I haven’t tried these (I don’t like buying gadgets), so I can’t comment on them .
I did find massaging my feet in various ways very helpful (besides there being no expenses involved). Here is one technique you can do in bed before getting up: Press your thumbs into the middle of your sole, and drag them apart towards the outer edges – to straighten out that plantar sheet as it were. You will find bumpier areas where the fascia is tigher. Work your way from the heel area to the toe base. You can use lotion or massaging, if you like (I did not find that necessary, though). Do experiment to find other massaging and kneading techniques that feel good to you. I enjoyed taking hold of my toes and bending them upwards with one hand, while supporting my foot with the other hand and gently massaging the fascia with my thumb (you can really feel that tough band in the arch area). Take about five minutes to do this – it feels good. It feels even better if you can get someone else to do it for you!
You could also do calf stretches using a belt or even a dog leash. Sit on the floor with your leg stretched out in front of you, loop the belt or leash’s loop around your toes and pull. Keep your knee straight, and hold for 30 seconds. You should be able to do this in bed, too. Check out “Doctor Jo”’s video for more visual instructions (see sources).
I also kept a golf ball in my bedside drawer to roll my feet on as soon as I swung them out of bed (golf balls are very hard). Doctor Jo suggests using one of those swimming noodles (you could save time by rolling both feet on them at once). You could also easily keep a golf ball, or cut-to-size swimming noodle in your office to use while working at a desk.
Dr Mandell recommends a frozen water bottle as the very best tool for releasing the plantar fascia. Lay your frozen water bottle on the floor, and roll your foot over it backwards and forwards, putting as much pressure on it as you can tolerate. Keep this up for a minute or two. Then pull your toes upward to stretch the fascia, and continue moving your foot back and forth over the bottle while pressing down on it. Continuing this movement, with your toes continuing to point up, put more pressure first on the outer side of your foot, then on the inner side (in other words, slowly roll your foot on the bottle from right to left). All of this should take about 3-4 minutes, and will actually feel quite good.
Now it’s time to stretch the fascia even more by taking hold of your toes with your hand and pulling them up towards your face. You feel more stretching at the bottom of your foot, in your Achilles tendon, and even in your calf. Hold for about 30 seconds.
To finish off the exercise release your foot and roll it once again over the water bottle, as in the beginning, for another minute. The pressure you apply is a kind of acupressure on that area. The ice in the bottle will also have a beneficial effect on the pain. Check out Dr Mandell’s video to get these instructions in a more visual manner (see sources).
Here is another exercise you can do to strech the fascia, the Achilles tendon as well as the calf all in one go. You can even do both feet at the same time. Find a firm step to stand on with the ball of your feet, while dipping your heels below the level of the step. Stairs work well, a sturdy step ladder will do, too. I like to bob up and down the curb along the streetside while waiting for a bus.
And one more secret little gem I discovered myself: After having walked on monotonously even concrete for a while until my feet ache it feels great to stand on a couple of big pebbles or even rocks that are the opposite of even. Experiment with different sizes and shapes and see what I mean!
In closing, I want to pass on the insight that our whole fascial system needs maintenance. Shortening of fascial tissue (with ensuing problems) can happen not only through irritation, but through inactivity as well. Think of the extra cellular matrix as a sponge, and the fasciae as the fibres of that sponge. The sponge absorbs water, and must be “wrung out” through body movement – so it can get rid of toxins, absorb fresh water and keep the watery extra-cellular environment clean. As Dr Mandell says, “no movement – no function”. The enemy of fasciae is extended bouts of stillness. Please note that I did not say “exercise” (as this sounds too strenuous for many people, and there is no need for strenuousness) – I said “movement”. Regular, daily movement through a wide range (which ever way you like to do it) will keep the circulation going and maintain the health and flexibility of fasciae well into old age.
Sources (besides my own experience):
Bristol Massage Clinic (March 1, 2018) Tight jaw? Tight hips! Retrieved on June 6th from https://bristolmassageclinic.co.uk/blog/
DailyHealthPost. (2020, March 30). 9 Things You Need to Know About Fascia, Your Body’s Invisible Second Skin. Retrieved on June 8th from https://dailyhealthpost.com/what-is-fascia/
Doctor Jo (2012, June 22). Plantar fasciitis stretches and exercises – Ask Doctor Jo. Retrieved on June 8th from https://www.youtube.com/watch?v=0PeVmTMdWhk
Footminders (2020). Pronation and Shoe Wear: Not What You Would Normally Think! Retrieved on June 8th from https://www.footminders.com/pages/pronation-and-shoe-wear
Mandell, A. (2017, Nov 5). Plantar fasciitis fast pain relief remedy (one ingredient: bottle water). Retrieved on June 6th from https://www.youtube.com/watch?v=dRffA-6Hza8
Mayo Foundation for Medical Education and Research (1998-2020). Plantar fasciitis. Retrieved on June 6th, 2020 at https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846
Schleip, R., Jäger, H., Klingler, W. (2012). What is ‘fascia’? A review of different nomenclatures. Journal of Bodywork & Movement Therapies (2012) 16, pp.496-502. Retrieved on June 6th from https://rolfing.org/wp-content/uploads/2017/09/Schleip2012_FasciaNomenclatures.pdf. DOI: http://dx.doi.org/10.1016/j.jbmt.2012.08.001
Wikipedia (17 November 2019). Plantar fascia. Retrieved on June 6th from https://en.wikipedia.org/wiki/Plantar_fascia



